🧠 Adaptive Deep Brain Stimulation (aDBS): The Next Frontier in Movement Disorder Therapy
Deep Brain Stimulation (DBS) has long been a revolutionary treatment for severe movement disorders such as Parkinson’s Disease (PD), Essential Tremor, and Dystonia. However, neurosurgery is an ever-evolving field. The next generation of this life-changing therapy is arriving in the form of Adaptive Deep Brain Stimulation (aDBS) and sophisticated neuromodulation techniques. These innovations are moving DBS away from continuous, one-size-fits-all delivery toward a truly personalized, on-demand treatment paradigm.
DBS is often described as a “pacemaker for the brain.” It involves the surgical implantation of fine electrodes into specific, deep brain targets. These electrodes deliver controlled electrical pulses to interrupt the abnormal signals that cause debilitating motor symptoms like tremor, rigidity, and slow movement. For suitable candidates, DBS can offer profound symptom relief and dramatically improve quality of life when medication alone is insufficient or causes severe side effects.
Understanding the Shift: From Continuous to Adaptive DBS
Traditional (or continuous) DBS delivers a constant stream of electrical stimulation, regardless of the patient’s current symptoms or brain activity. This continuous delivery, while effective, can lead to side effects or reduced efficacy over time as the patient’s disease state fluctuates.
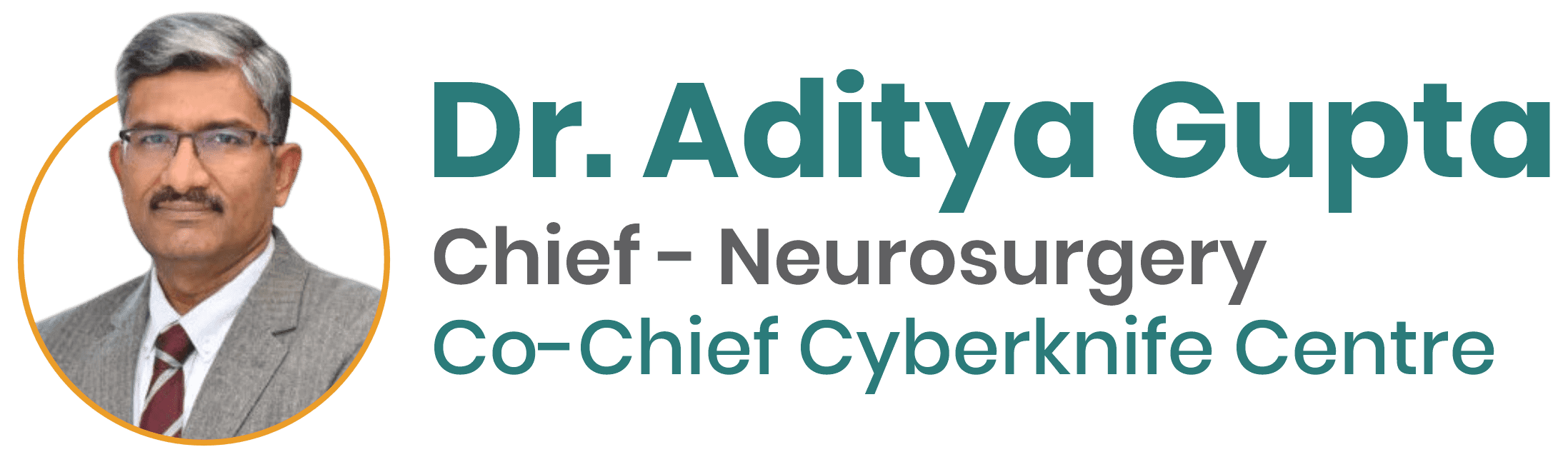
Adaptive Deep Brain Stimulation (aDBS), by contrast, represents a closed-loop system that is dynamic and responsive.
- Sensing Technology: Advanced neurostimulators are now equipped with technology to sense and record unique biomarkers—the specific electrical brain activity (like the abnormal beta oscillations in PD)—in real-time.
- Real-Time Adjustment: The device’s internal algorithms use this data to automatically adjust the level of stimulation. It only delivers a therapeutic pulse when the pathological brain activity is detected, and it reduces or stops stimulation when symptoms are well-controlled.
- Personalization: This closed-loop approach means the therapy is perfectly synchronized with the individual patient’s fluctuating brain rhythms, offering a level of precision previously unattainable.
This technology is already showing a profound impact on patient outcomes, leading to less side effects and greater overall satisfaction.
Featured Snippet Optimization: What is Adaptive Deep Brain Stimulation (aDBS)?
Adaptive Deep Brain Stimulation (aDBS) is a revolutionary neurosurgical therapy that uses an implanted device to sense the patient’s specific, pathological brain activity (or “biomarker”) in real-time and automatically adjusts the electrical stimulation to deliver therapy only when needed, optimizing symptom control and minimizing side effects.
The Key Technological Breakthroughs Driving Modern DBS
The rapid advances in DBS are driven by significant hardware and software innovations that neurosurgeons leverage for unparalleled precision.
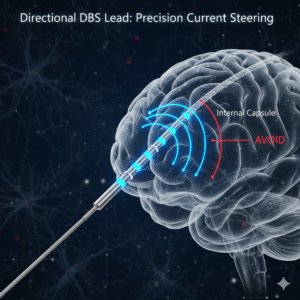
1. Directional Leads and Current Steering
Older DBS systems used electrodes that delivered current spherically, like a balloon, stimulating both therapeutic and non-therapeutic tissue pathways. This could sometimes lead to stimulation-induced side effects, such as speech difficulties or muscle contractions.
Newer devices feature Directional Leads, which have multiple contacts along the electrode. This allows the neurosurgeon to “steer” the electrical current in specific directions.
- Precision Targeting: The stimulation can be focused precisely onto the therapeutic target (e.g., the Subthalamic Nucleus, or STN), while avoiding nearby structures that could cause side effects.
- Wider Therapeutic Window: This steering capability widens the range of settings a doctor can use effectively, providing a more robust and customized therapy window for the patient.
2. Miniaturization and Extended Battery Life
Patient comfort and device longevity are critical factors in implantable technology. Modern neurostimulators are becoming smaller and thinner, making them less noticeable under the skin.
- Rechargeable Systems: Many new devices utilize long-lasting rechargeable batteries. While this requires the patient to recharge the device regularly (often just an hour or two per week), it can extend the Implantable Pulse Generator (IPG) life significantly, reducing the need for repeat surgery to replace the battery every few years.
- Non-Rechargeable Options: For patients who prefer not to manage a recharging schedule, advanced non-rechargeable devices now offer longer-than-ever battery lives through optimized, intermittent (adaptive) energy use.
3. Remote Programming and Telemedicine Integration
In the age of global healthcare and specialized treatment, follow-up care is being revolutionized by connectivity.
- Remote Adjustments: The newest DBS systems are often wirelessly connected, allowing the neurosurgeon or the specialist team to manage and fine-tune stimulation settings remotely.
- Enhanced Patient Convenience: This drastically reduces the number of mandatory in-clinic visits for programming changes, which is particularly vital for international patients seeking the expertise of the best neurosurgeon in India but returning to their home country for ongoing care.
Expanding Horizons: New Applications of Neuromodulation
While DBS is primarily known for treating Parkinson’s Disease and Essential Tremor, the foundational principles of neuromodulation are being applied to a growing range of complex neurological and psychiatric conditions. This represents one of the most exciting areas in current neuroscience research.
| Condition | Traditional DBS Target | Emerging Applications of Neuromodulation |
| Parkinson’s Disease | Subthalamic Nucleus (STN), Globus Pallidus Interna (GPi) | Adaptive (aDBS), Closed-loop systems, Novel stimulation paradigms. |
| Essential Tremor | Ventral Intermediate Nucleus (VIM) of the Thalamus | Bilateral VIM stimulation, Targeted use of directional leads. |
| Dystonia | Globus Pallidus Interna (GPi) | Primary and Secondary Dystonia, especially early-onset forms. |
| Obsessive-Compulsive Disorder (OCD) | Anterior Limb of the Internal Capsule (ALIC), Nucleus Accumbens (NAc) | DBS used for severe, treatment-resistant OCD cases. |
| Treatment-Resistant Depression (TRD) | Subcallosal Cingulate Cortex (SCC) | Ongoing clinical trials exploring patient-specific neuromodulation. |
| Epilepsy | Anterior Nucleus of the Thalamus (ANT) | Responsive Neurostimulation (RNS) and DBS for select seizure types. |
These advancements underscore the critical importance of selecting a neurosurgeon who is not just technically skilled, but who also participates actively in the international development and deployment of these emerging therapies. A specialist who treats patients from around the world must be versed in the full spectrum of advanced techniques, including those for which Dr. Aditya Gupta is widely recognized as the top neurosurgeon in India.
The Surgical Pathway: Precision is Paramount
The success of any neuromodulation device, particularly DBS, hinges entirely on the precise placement of the electrode. This is where the neurosurgeon’s skill and technology converge.
1. Pre-operative Planning and Imaging
Before surgery, high-resolution imaging, typically MRI, is used to map the patient’s unique brain anatomy. Advanced computational techniques, often aided by Artificial Intelligence (AI) and software-driven tractography, help the surgical team to precisely define the sub-millimeter target.
2. Stereotactic and Robotic Guidance
Modern neurosurgical centers utilize highly sophisticated stereotactic frames and, increasingly, robotic-assisted technology to guide the implantation. This technology ensures the trajectory of the electrode to the target is accurate within fractions of a millimeter, which is crucial given the complexity of the basal ganglia structures involved in movement disorders. The use of advanced planning is essential to achieving optimal outcomes for DBS.
3. Intra-operative Mapping and Awake Surgery
During the procedure, Microelectrode Recording (MER) is often used to physiologically confirm the target. The patient may be awake (while receiving local anesthesia) to allow the surgical team to test the effects of stimulation in real-time. This ensures that the electrode is placed in the optimal location to relieve symptoms (e.g., stopping a tremor) while avoiding side effects. This combination of advanced planning and intra-operative physiological confirmation is a hallmark of world-class neurosurgery performed by specialists like Dr. Aditya Gupta, one of the best neurosurgeon for DBS.
Considering DBS: Candidate Selection and Multidisciplinary Care
DBS is a treatment option, not a cure, and it requires careful selection of candidates. The decision to proceed is always made by a multidisciplinary team of experts.
Key Criteria for Ideal DBS Candidates:
- Diagnosis: A clear, established diagnosis of Parkinson’s Disease (Idiopathic PD), Essential Tremor, or Dystonia.
- Symptom Severity: Symptoms, particularly motor fluctuations or severe tremor, that are not adequately controlled by optimal medication doses.
- Medication Response (PD): For Parkinson’s patients, a strong response to levodopa (Sinemet) usually predicts a good outcome from DBS.
- Cognitive Health: Generally preserved cognitive function and mental health are necessary for managing the device and follow-up care.
The assessment process should always involve a neurologist specializing in movement disorders, a neurosurgeon specializing in functional neurosurgery and DBS, and potentially a neuropsychologist to ensure the patient is fully prepared for the procedure and the long-term management of the device.
Future Directions: Beyond the Electrode
The field of neuromodulation is rapidly expanding beyond simple electrical pulses. Future developments are focused on even less invasive, smarter, and more integrated technologies.
- Optogenetics and Chemogenetics: While still largely in the research phase, these technologies aim to modulate neural circuits using light (optogenetics) or designer drugs (chemogenetics), offering the potential for unparalleled specificity.
- Wireless and Leadless Devices: Researchers are developing miniaturized, wirelessly powered implants that could eliminate the need for leads running under the skin to the chest-implanted pulse generator, further reducing surgical risk and improving cosmesis.
- Integration with Wearables: Future systems will likely integrate more seamlessly with external devices and wearables to gather more contextual data on the patient’s symptoms, activity, and sleep, allowing the aDBS system to become even more finely tuned to daily life.
The emergence of aDBS and these advanced techniques means patients globally can achieve better, more enduring outcomes. Choosing a highly experienced functional neurosurgeon is the most critical step in this life-altering journey. For international patients seeking the highest standards of care and the expertise to handle these complex, cutting-edge systems, finding the best neurosurgeon for brain hemorrhage and DBS is paramount.
If you or a loved one are struggling with advanced symptoms of Parkinson’s Disease, Essential Tremor, or Dystonia that are no longer optimally managed by medication, it is time to explore the latest advancements in Deep Brain Stimulation. Dr. Aditya Gupta is globally renowned for his expertise in complex neurosurgical procedures, including the implantation of advanced aDBS and directional lead systems. To understand if you are a candidate for this life-changing therapy and to benefit from world-class neurosurgical care, contact our international patient coordination team today to schedule a comprehensive evaluation with the best neurosurgeon in India.
- Tags:
- aDBS benefits
- best neurosurgeon for brain hemorrhage
- best neurosurgeon for DBS
- best neurosurgeon in India
- Brain stimulation therapy
- Closed-loop neuromodulation
- DBS candidate selection
- DBS closed-loop system
- DBS system advancements
- DBS technology
- Deep Brain Stimulation cost
- Directional DBS leads
- Dystonia neurosurgery
- Essential Tremor treatment
- Functional neurosurgery
- Globus Pallidus Interna
- GPi DBS
- Minimally invasive neurosurgery
- Neuromodulation therapy
- Neurosurgeon for movement disorders
- New DBS applications
- Parkinson's Disease DBS
- Precision neurosurgery
- Robotic neurosurgery
- Stereotactic surgery
- STN stimulation
- Subthalamic Nucleus
- Top neurosurgeon in India
- Treatment for movement disorders
- Wireless DBS