Aneurysms are like silent time bombs that exist within our bodies. They are weakening spots in the walls of blood arteries that can blow out and burst, causing serious consequences or even death if not addressed. Aneurysm Surgery in Gurgaon becomes necessary when the danger of rupture is considerable to avoid catastrophic effects and restore health.
Let us go more into this important component of vascular health.
What are Intracranial Aneurysms?
Intracranial aneurysms are localized pathological dilatations of cerebral arteries. Most intracranial aneurysms are saccular or berry aneurysms, whereas dissecting, fusiform, infectious, traumatic, and oncotic aneurysms are much rarer.
Saccular, or berry aneurysms, correspond to lobulated focal outpouchings of the wall of the arteries of the circle of Willis. Current opinions suppose that intracranial aneurysms result from a combination of hemodynamic stresses and acquired degenerative changes within the arterial wall

What Does an Aneurysm Look Like
Aneurysms may present as:
- Rupture of the fragile wall of such aneurysms mostly causes subarachnoid haemorrhage (SAH), which patients describe as “the worst headache of their life.”
- The mass effect causes cranial nerve problems.
- Asymptomatic, discovered unintentionally during imaging for other purposes.
- It is estimated that around 3% to 5% of the population has an intracranial aneurysm.
- Subarachnoid haemorrhage induced by the rupture of an intracranial aneurysm accounts for one out of every twenty strokes.
Because the disease hits at a young age and is frequently deadly, the loss of productive life years is comparable to that of a cerebral infarction or intracranial haemorrhage
Complications Of SAH
Many people do not survive the first bleed or get substantial brain impairment as a result of it. Those who survive have a significant risk of recurrent bleeding, which can be deadly in 70-80% of instances. Even if the aneurysm is repaired before rebleeding, 15% of patients who survive the initial haemorrhage have ischemic strokes or die as a result of cerebral vasospasm. Non-neurological complications are common in people with SAH.
These include fever, anaemia, hypertension and hypotension, hyperglycemia, hypernatremia/hyponatremia, hypomagnesaemia, heart failure and arrhythmias, as well as pulmonary oedema and pneumonia. As a result, these patients require intense care management to avoid and treat such complications
Pituitary Adenoma Tumor:
- In cases of suspected SAH, a CT scan should be conducted. However, CT can be negative in rare circumstances, especially if performed many days after the occurrence.
- Although MR is highly sensitive when conducted correctly and evaluated by a competent radiologist, SAH is commonly overlooked.
- Patients with SAH should undergo selective cerebral angiography to identify aneurysms and their anatomical characteristics.
- When traditional angiography cannot be conducted in a timely manner, MR or CT angiography may be used instead.
What Are The Management Recommendations
Surgery (Clipping) V/s Embolization (Coiling)
Aneurysm Surgery in Gurgaon has been the traditional means of treating aneurysms. The aneurysm, parent vessel(s), and surrounding structures are all exposed directly during Aneurysm Surgery in Gurgaon. The aneurysm is then secured with a silver clip placed along the neck, restricting it from circulation. Surgery has the disadvantage of being intrusive and causing harm to the normal brain parenchyma
Another therapeutic option by Artemis’ AVM Surgeon in Gurgaon is endovascular embolization (coiling) of aneurysms. In this procedure, a microcatheter is inserted into the aneurysm via one of the leg arteries and blocked with coils (typically detachable platinum coils) to prevent further bleeding. Advantages: Because coiling is a less invasive method, it is less likely to cause brain parenchymal harm.
International Subarachnoid Aneurysm Trial Study (Isat)
1. Randomized, prospective, worldwide controlled study. In aneurysms that were judged eligible for either therapy, we compared a neurosurgical cutting policy to an endovascular treatment program.
2. 9559 patients were screened; 2143 (22.4%) were randomized, and the difference in the risk of dependence or mortality between the two groups was assessed.
3. Results: At one year, the coiling group had a significantly better result than surgical patients, with a relative risk reduction of 22.6%.
4. The early survival advantage was sustained for up to seven years.
5. Endovascular therapy was found to reduce the risk of epilepsy in individuals significantly. The risk of late rebleeding was somewhat increased (0.16%). Despite a low chance of rebleeding, the coiling group had a superior result.
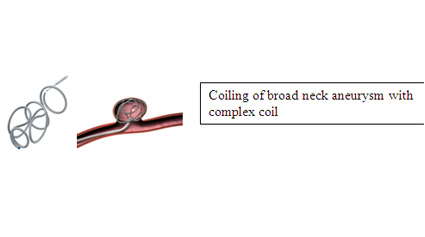
Are Broad Neck Aneurysms Suitable For Coiling
The majority of broad neck aneurysms are treated with coils, including 3D and complex coils. These coils remain stable even in broad neck aneurysms. SAH is a medical emergency that is commonly misdiagnosed. In individuals with an acute onset of severe headache, there should be a strong suspicion of SAH.
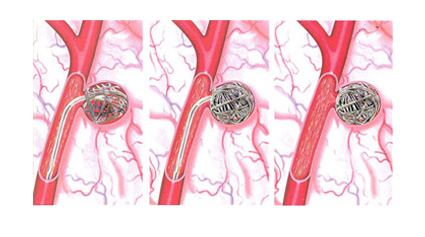
Patients with SAH should be handled in the ICU with adequate neuroaesthetics support and treatment. To avoid repeated bleeding, aneurysms should be treated early on. Some patients require balloon assistance or stent implantation. Balloon-aided coiling for broad neck aneurysms: A balloon is temporarily inflated at the aneurysm’s neck to hold the coils in place.
Stent-assisted coiling of wide neck aneurysm: a stent is put across the neck of a broad neck aneurysm to hold the coils and rebuild the artery.
What Are Flow Diverters When Do We Use It
Flow diverter is a stent with a tighter wire mesh and hence reduced porosity. Flow diversion is an endovascular procedure in which a device is inserted in the parent blood artery to redirect blood flow away from the aneurysm rather than inside the aneurysm sac, as is the case with coiling.
This procedure is utilized to treat enormous wide-necked aneurysms, as well as extremely minor burst blister aneurysms. Blood flow to the aneurysm sac is decreased almost immediately after stent deployment, and the aneurysm closes completely within six weeks to six months following the treatment. The flow diverter maintains normal blood circulation while providing permanent long-term blockage.
QUICK CONTACTS
- Phone : +91-9910094615
- Email : dradityaguptaofficial@gmail.com
-
Address : Artemis Hospitals Sector 51 Gurgaon, Haryana, 122001, India
LOCATION
- Copyright 2023 Dr. Aditya Gupta. All Rights Reserved.

